
Allergic Conjunctivitis
Allergic conjunctivitis is the most common immune response of the eye, affecting approximately 25% of the general population and 30% of children, who suffer with allergies.
In this article you will find information about the following:
What is Allergic Conjunctivitis?
Allergic conjunctivitis is the most common immune response of the eye, affecting approximately 25% of the general population and 30% of children, who suffer with allergies. It is caused by direct exposure of the surfaces of the eye to environmental allergens.
What are the common symptoms of Allergic Conjunctivitis?
Most common symptom is variable itching of the eyes, rather than pain, with increased watering. Clinical signs include redness all around the white of the eye that may progress to swelling and profuse watery discharge.(Fig 1)
Fig: Allergic conjunctivitis.
Arrow indicates area of chemosis in the conjunctivitis.
(From Adkinson NF Jr, Bochner BS, Burks AW, et al, editors: Middleton's allergy: principles & practice, ed 8, vol 1, St Louis, Mosby/Elsevier, 2014, p 619.)

When do I get the Allergic Conjunctivitis and what triggers it?
Allergic conjunctivitis occurs in a seasonal or, less frequently, perennial form.
Seasonal allergic conjunctivitis is typically associated with allergic rhinitis ( Nasal Allergy) and is most commonly triggered by pollens. Major pollen groups in the temperate zones include trees (late winter to early spring), grasses (late spring to early summer), and weeds (late summer to early fall), but seasons can vary significantly in different parts of the world. Mold spores can also cause seasonal allergy symptoms, principally in the summer and fall. Seasonal allergy symptoms may be aggravated by coincident exposure to perennial allergens.
Perennial allergic conjunctivitis is triggered by allergens such as animal danders (dry skin shed by animals) or dust mites that are present throughout the year, in beddings, carpets and all around the house. Symptoms are usually less severe than with seasonal allergic conjunctivitis. Because pollens and soil molds may be present intermittently by season, and exposure to allergens such as furred animals may be perennial, classification as intermittent (symptoms present <4 days/wk or for <4 wk) and persistent (symptoms present >4 days/wk and for >4 wk) has been proposed.
What are the other types of Allergic Conjunctivitis?
-
Vernal Keratoconjunctivitis
Vernal keratoconjunctivitis is a severe form of allergic conjunctivitis that affects both eyes and causes inflammation of the delicate mucosa of the inside of the Upper lids. It may threaten eyesight if there is corneal involvement. Although vernal keratoconjunctivitis is not a true allergic reaction, it occurs most frequently in children with seasonal allergies, asthma, or atopic dermatitis.
Vernal keratoconjunctivitis affects boys twice as often as girls and is more common in people of Asian and African descent. It affects primarily children in warm temperate areas, with exacerbations in the spring and summer, but can occur throughout the year.
What are the Signs and Symptoms?
They include severe ocular itching exacerbated by exposure to irritants, light, or perspiration. In addition, patients may complain of severe photophobia (glare to light), foreign body sensation, and watering from the eyes.
Giant lumps (aka papillae) occur predominantly on the inside of the upper lid and are typically described as cobblestoning.(Fig 2) Other signs include a stringy or thick, ropey discharge, cobblestone papillae, transient yellow-white points in the limbus (known as Trantas dots) and on the conjunctiva (known as Horner points). The Cornea can scar up by constantly rubbing on it from the lumpy cobblesones due to repeated blinking and can cause permanent damage. Children with vernal keratoconjunctivitis have measurably longer eyelashes, which may represent a reaction to ocular inflammation.
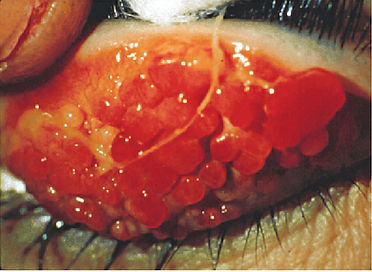
Fig 2: Vernal keratoconjunctivitis.
Cobblestone papillae and ropey discharge are seen on the underside (tarsal conjunctiva) of the upper eyelid.
(From Adkinson NF Jr, Bochner BS, Burks AW, et al, editors: Middleton's allergy: principles & practice, ed 8, vol 1, St Louis, Mosby/Elsevier, 2014, p 627.)
·Atopic Keratoconjunctivitis
Atopic keratoconjunctivitis is another chronic inflammatory ocular disorder most often involving the lower lids and mucosa. It may threaten eyesight if there is corneal involvement. Almost all patients have atopic dermatitis (allergy on the skin), and a significant number have asthma. Atopic keratoconjunctivitis rarely presents before late adolescence. Symptoms include severe bilateral itching, burning, photophobia, and tearing with a mucoid discharge that are much more severe than in allergic conjunctivitis and persist throughout the year. The conjunctival mucosa is injected and chemotic. Trantas dots or giant papillae may also be present. Eyelid eczema can extend to the periorbital skin and cheeks with erythema and thick, dry scaling. This can predispose your eyelids to get blepharitis ( bacterial infection of the lids) is common because of eyelid induration and maceration.
Chronicity of the above diseases (Vernal and atopic) can lead to early clouding of the natural lens. (known as Cataract) and also predispose the cornea to change shape and become very irregular (keratoconus).
·Giant Papillary Conjunctivitis
Giant papillary conjunctivitis has been linked to chronic exposure to foreign bodies, such as contact lenses, both hard and soft, ocular prostheses, and sutures. Symptoms and signs include mild bilateral ocular itching, tearing, a foreign body sensation, and excessive ocular discomfort with mild mucoid discharge with white or clear exudate on awakening, which may become thick and stringy. Trantas dots, limbal infiltration, bulbar conjunctival hyperemia, and edema may develop.
·Contact Allergy
Contact allergy typically involves the eyelids but can also involve the conjunctivae. It is being recognized more frequently in association with increased exposure to topical medications, contact lens solutions, and preservatives.
What is the Treatment of Allergic Conjunctivitis?
Primary treatment of ocular allergies includes avoidance of allergens, cold compresses, and lubrication.
-
Avoid allergens: Identify the specific allergens that trigger your symptoms and take steps to avoid them. Common allergens as discussed above include pollen, dust mites, pet dander, mold spores, and certain foods. Monitor pollen forecasts and stay indoors when pollen counts are high. Use air purifiers and allergen-proof covers for your bedding and pillows.
-
Keep windows closed: Keep windows and doors closed during peak allergy seasons to prevent pollen and other outdoor allergens from entering your home. Use air conditioning with high-efficiency particulate air (HEPA) filters to filter the air inside your home.
-
Minimize outdoor exposure: Limit your time outdoors when allergen levels are high. Stay indoors during early mornings and evenings when pollen counts are usually at their highest. If you do go outside, wear sunglasses and a hat to protect your eyes and face from pollen. You can use Vaseline and rub at the nasal entry points and around the eyelashes to prevent the pollens from stimulating the immune system.
-
Practice good hygiene: Wash your hands frequently (especially after being outdoors) to remove any allergens that may have settled on your skin. Shower and change your clothes after spending time outside to remove pollen from your hair and clothing.
-
Clean your home regularly: Keep your living environment clean to minimize allergen exposure. Vacuum regularly using a vacuum cleaner with a HEPA filter to trap allergens. Dust surfaces with a damp cloth and remove carpets or rugs if possible, as they can harbour allergens.
-
Manage indoor humidity: Keep indoor humidity levels between 30% and 50% to discourage the growth of mould and dust mites. Use dehumidifiers or air conditioners to control humidity. Fix any leaks or water damage promptly.
-
Avoid smoking and second-hand smoke: Smoking and exposure to second hand smoke can worsen allergy symptoms. Quit smoking if you're a smoker and avoid being around others who smoke.
Secondary treatment
The regimens include the use of oral or topical antihistamines and, if necessary, topical decongestants, mast cell stabilizers, and anti-inflammatory agents. Drugs with dual antihistamine and mast cell–blocking activities provide the most advantageous approach in treating allergic conjunctivitis, with both fast-acting symptomatic relief and disease-modifying action. Children often complain of stinging or burning with use of topical ophthalmic preparations and usually prefer oral antihistamines for allergic conjunctivitis. It is important not to contaminate topical ocular medications by allowing the applicator tip to contact the eye or eyelid. Using refrigerated medications may decrease some of the discomfort associated with their use. You are better off seeing your local GP or consult an eye specialist (Ophthalmologist), who can treat the condition more appropriately as sometimes treatment of ocular allergy includes topical (or rarely oral) corticosteroids or stronger immune-modulator medications.
C
Mr Rana’s care of me has been excellent. He has explained things very clearly and performed the surgery expertly and quickly. I have complete faith in him and look forward to him continuing to be available to monitor my needs.
S.Q
I would without hesitation recommend Mr Rana. His knowledge & experience of complex corneal conditions is unparalleled. He always seeks to explain options, risks, expected outcomes & timescales. I trust him implicitly to provide the best possible care and outcome for my condition
W.H
Mr. Rana is a Consultant Surgeon with whom I have had the greatest confidence in since our initial interaction a few years ago. He has instilled a lot of confidence in me moving forward with my eye care & I am extremely grateful. I have & would definitely recommend Mr Mrinal Rana
Don't take our word for it!
Reviews from happy patients

